One of the most empowering parts of motherhood is learning to be confident in owning your experiences. You research topics and become educated so you can make informed decisions that are right for [your] family. What is right for [you] won’t necessarily be right for those around you, and that’s okay. Birth is not black and white. There are many paths.
My mom often says, “You need to ask the right questions to get the right answers.” We often seek answers in life without evening knowing what question to ask!
If you are considering scheduling an induction, you first need to know this question: “What is my Bishop Score?”
So, what IS a bishop score? A Bishop Score is a mathematical formula care providers use to determine the favorability of the cervix for an induction. To accumulate this score, your care provider will need to begin by doing a cervical exam. (*Side note: Every time you receive a cervical check, you are introducing bacteria into your vagina. It increases the potential risk for infection.)
During this exam, your care provider will check for the following:
Cervical dilation – the opening of the cervix, the entrance to the uterus, during childbirth.
 Cervical effacement – refers to a thinning of the cervix.
Cervical effacement – refers to a thinning of the cervix.
 Cervical consistency – how firm, intermediate or soft the cervix is
Cervical consistency – how firm, intermediate or soft the cervix is
 Cervical position – if the cervix is posterior, intermediate or anterior
Cervical position – if the cervix is posterior, intermediate or anterior
“The position of the cervix varies between individual women. As the anatomical location of the vagina is actually downward facing, anterior and posterior locations relatively describe the upper and lower borders of the vagina. The anterior position is better aligned with the uterus, and therefore there is an increased likelihood of spontaneous delivery.” – Wiki
Fetal station – refers to how far down the baby’s head has descended into the mother’s pelvis. Fetal station describes the position of the fetus’ head in relation to the distance from the ischial spines.
 Each component is given a score of 0-2 or 0-3.
Each component is given a score of 0-2 or 0-3.

A score of 5 or below indicates the woman is unlikely to go into spontaneous labor at that time. An induction is likely to fail and result in a cesarean.
A result of 8 or more indicates that an induction is more than likely to succeed in a vaginal birth.
A result of 9 or more indicates the woman will likely go into labor on her own very soon.
Modified Score:
An extra point is added for moms who have pre-eclampsia and for each previous vaginal delivery.
A point is subtracted for a pregnancy being post-date, no previous vaginal deliveries or premature pre-term rupture of membranes.
It is important to also consider where you are in relation to your due date. ACOG recently redefined their guidelines for Term Pregnancies. An expecting mom is no longer considered Full Term until 39 weeks – 40 weeks + 6 days. The days of inducing babies for non-medical reasons at 37 weeks is coming to an end. The studies show it’s simply not a good idea.
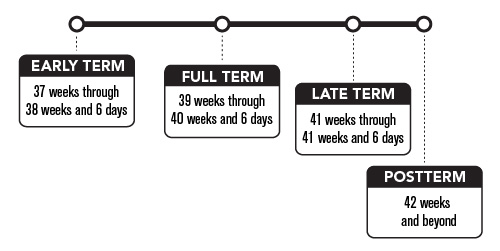
“Gestation in singleton pregnancies lasts an average of 40 weeks (280 days) from the first day of the last menstrual period to the estimated date of delivery. In the past, the period from 3 weeks before until 2 weeks after the estimated date of delivery was considered “term” (1), with the expectation that neonatal outcomes from deliveries in this interval were uniform and good. Increasingly, however, research has identified that neonatal outcomes, especially respiratory morbidity, vary depending on the timing of delivery even within this 5-week gestational age range. The frequency of adverse neonatal outcomes is lowest among uncomplicated pregnancies delivered between 39 0/7 weeks of gestation and 40 6/7 weeks of gestation. For this reason, quality improvement projects have focused, for example, on eliminating nonmedically indicated (induced) deliveries at less than 39 0/7 weeks of gestation.” –ACOG
What other factors might hinder a successful induction?
Position. Position. Position.
Do you know the difference in occiput anterior and occiput posterior? (If not, I hope you have a doula!)
Occiput anterior– Back of the head towards mother’s belly; baby looking at mother’s back.
Occiput posterior– Back of the head towards mother’s back; baby looking at mother’s belly.

Have you ever heard of a woman who complained of excruciating back pain in labor? That was more than likely due to a posterior baby. Ouch! It is extremely important to be proactive about encouraging proper position in pregnancy. Seeing a Webster Certified Chiropractor is a MUST in pregnancy. Find one HERE. It is also important to encourage optimal fetal positioning by being aware of your posture and doing your daily/weekly exercises. Plain and simple: A posterior baby’s head does not put the necessary pressure on the cervix to encourage change. Learn how to recognize a posterior position and then encourage baby to turn!
Our national cesarean rate is 33.3% – that is an alarmingly high number. If you, your best friend and I were to walk into the hospital right now, one of us would be walking out with a surgical birth. The Coalition for Improving Maternity Services designates and recognizes Mother Friendly Hospitals for their excellence in practicing and promoting Evidence-Based care. To receive this designation, they recommend that the cesarean and VBAC rates are as follows:
- Has a total cesarean rate of 10% or less in community hospitals, and 15% or less in tertiary care (high-risk) hospitals;
Has a VBAC (vaginal birth after cesarean) rate of 60% or more with a goal of 75% or more.
Compare that to our national cesarean rate and you can see a big difference. Ask your care provider what his/her cesarean rate is — or find your hospital’s rate under your listed state HERE. And also ask what his/her VBAC rate is. If your care provider is going to induce you with pitocin, ask them how they normally use it and what restrictions, if any, that might put on you. I’ve seen several successful inductions where Evidence Based care providers used pitocin the way it should be when moms need a bit of help getting things going. They turned the pitocin on and left it going in small doses (2 gradually increased to 8 mUnit) and then turned it off and disconnected the IV when mom started to labor on her own. Many of my doula clients have had beautiful natural water births in the hospital after a medically necessary induction. (Darn you pre-eclampsia!)
Last but not least, ask yourself why you are considering induction. If not for a medical reason, does the risk outweigh the benefit? Does your care provider appear to be pressuring you to induce? Talk to them and voice your concerns. Become an active participant in your care. (And if they aren’t willing to reason, don’t be afraid to switch to a new care provider. It’s only to late once the baby is in your hands!) …Or are you just feeling over and done with pregnancy? If so, that is completely normal. We all start to feel that way. The waiting game is hard, but an induction can be even harder.
This birth that you are planning right now greatly effects your future births. Consider your options carefully. I hope this has helped you find what questions to ask so you can find the answers that you need to make the right decision for you.Happy Birthing! (and CONGRATULATIONS!)
-Laney Sweet | DFW Birth Doula | The Birthing Tree | http://www.LaneySweet.com
Great Synopsis, Laney!
Great information regarding the bishop score! I will definitely be referring to that quite frequently. I would love to hear some more regarding induction in multiples pregnancy (ie. twins triplets quads) in the future.
Thanks for the excellent read!
Having an induction on or before your due date is so common and most women don’t know the full spectrum of risks associated with a non-medically needed induction. Thank you for sharing information on this important topic!
Great post! Your mom sounds like a smart lady. Great synopsis of what to consider before being induced.
Thank you so much for sharing! I’ll have to share this link on my blog. I really love the photos and diagrams…they’re very helpful. I just had a friend message me about her OB and how she kept pushing for an induction and all these different interventions. Ultimately she ended up firing the OB and went into labor naturally! :0 This just happened over the weekend 🙂